UAB announces first clinical-grade transplant of gene-edited pig kidneys into brain-dead human

UAB's xenotransplant team assisted with a groundbreaking study that may help hundreds of thousands of patients who need an organ transplant. UAB researchers recently tested the first human preclinical model for transplanting genetically modified pig kidneys into humans. The study's positive results could address the worldwide organ shortage. (UAB)
The UAB Marnix E. Heersink School of Medicine has announced the first peer-reviewed research outlining the successful transplant of genetically modified, clinical-grade pig kidneys into a brain-dead human, replacing the recipient’s kidneys. These positive results demonstrate how xenotransplantation could address the worldwide organ shortage crisis.
In a study published in the American Journal of Transplantation, UAB researchers tested the first human preclinical model for transplanting genetically modified pig kidneys into humans. The study recipient had two genetically modified pig kidneys transplanted in his abdomen after his native kidneys were removed. The organs were procured from a genetically modified pig at a pathogen-free facility.
For the first time, the kidneys transplanted were taken from pigs that had been genetically modified with 10 key gene edits that may make the kidneys suitable for transplant into humans. This process demonstrates the long-term viability of the procedure and how such a transplant might work in the real world. The transplanted kidneys filtered blood, produced urine and, importantly, were not immediately rejected. The kidneys remained viable until the study was ended, 77 hours after transplant.
“This game-changing moment in the history of medicine represents a paradigm shift and a major milestone in the field of xenotransplantation, which is arguably the best solution to the organ shortage crisis,” said Dr. Jayme Locke, director of the Comprehensive Transplant Institute in UAB’s Department of Surgery and lead surgeon for the study. “We have bridged critical knowledge gaps and obtained the safety and feasibility data necessary to begin a clinical trial in living humans with end-stage kidney failure disease.”
(UAB videography by Jeff Myers and Steve Wood)
Gene editing in pigs to reduce immune rejection has made organ transplants from pigs to humans possible, which could help thousands of people who face organ failure, disease or injury. The natural lifespan of a pig is 30 years; they are easily bred and can have organs of similar size to humans.
Genetically modified pig kidneys have been extensively tested in nonhuman primates. In addition to testing in primates, evaluating pig kidneys in a human preclinical research may provide information about the safety and efficacy of kidneys in humans, including in clinical trials.
“This human preclinical model is a way to evaluate the safety and feasibility of the pig-to-nonhuman primate model, without risk to a living human,” Locke added. “Our study demonstrates that major barriers to human xenotransplantation have been surmounted, identifies where new knowledge is needed to optimize xenotransplantation outcomes in humans, and lays the foundation for the establishment of a novel preclinical human model for further study.”
(UAB videography by Jeff Myers and Steve Wood)
The effort is supported by biotechnology pioneer United Therapeutics Corp., which awarded a grant to UAB to launch the innovative xenotransplantation program. Revivicor Inc., a subsidiary of United Therapeutics, provided the genetically modified pig that was the source of the investigational kidneys.
“All of us at Revivicor are in awe of the historic achievements at UAB with our investigational 10-gene xenokidney, or UKidney,” said David Ayares, chief scientific officer of Revivicor and a trailblazing genetic engineer since his early work cloning pigs. “We feel confident that this UKidney may turn out to be a lifesaving solution for thousands of people on dialysis, subject to successful completion of our clinical trials and achievement of FDA approval in the next several years.”
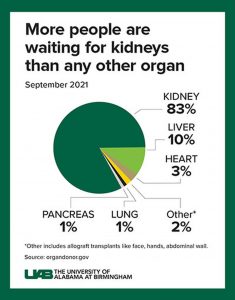
(UAB graphic by Jody Potter)
The peer-reviewed research is a study of ambitious scope and great significance, given that more than 800,000 Americans are living with kidney failure. Most never make it to the waiting list, and far too few human organs are available to put a dent in that number. Although dialysis can sustain life for some time, transplantation offers a better quality of life and a longer life for the few people who gain access to transplantation. Each stage of the xenotransplant study approximated the steps that might be taken in a Phase I clinical trial:
- The kidneys were removed from a donor pig housed at a pathogen-free, surgically clean facility. The kidneys were stored, transported and processed for implantation, just as human kidneys are.
- Before surgery, the brain-dead recipient and donor animal underwent a crossmatch compatibility test to determine whether the genetically modified pig kidney and its intended recipient were a good tissue match. A crossmatch is done for every human-to-human kidney transplant; however, this pig-to-human tissue-match test was developed at UAB and marked the first time a prospective crossmatch has been validated between the two species.
- The pig kidneys were placed in the anatomic locations for human donor kidneys, with the same attachments to the renal artery, renal vein and ureter that carries urine from the kidney to the bladder.
- The brain-dead recipient received standard immune-suppression therapy used in human-to-human kidney transplants.
The study was conducted to meet the standards that would apply to a Phase I human clinical trial, mirroring every step of a transplant between humans. It included approvals by an Institutional Review Board and Institutional Animal Care and Use Committee, a tissue compatibility confirmation, the standard procedures of human-to-human transplants to remove, preserve, transport and transplant kidneys, and giving the standard immunosuppression therapy to the recipient.
Learn more about the study here.
Transplant recipient helps open doors to future of organ transplantation
This scientific and medical breakthrough would not have been possible without Jim Parsons, the recipient, or his family.
Parsons, 57, was a registered organ donor through Legacy of Hope, Alabama’s organ procurement organization, and he had longed to have his organs help others upon his death; but his organs were not suitable for donation. His family permitted UAB to maintain Parsons on a ventilator to keep his body functioning during the study. His kidneys were removed and pig kidneys were transplanted.
“Mr. Parsons and his family allowed us to replicate precisely how we would perform this transplant in a living human. Their powerful contribution will save thousands of lives, and that could begin in the very near future,” Locke said. “Mr. Parsons’ gift honors his legacy and firmly establishes the viability, safety and feasibility of this preclinical model. Because of his gift, we have proposed this to be known as ‘The Parsons Model.’”
Parsons’ ex-wife, Julie O’Hara, and their children, Ally, David and Cole, made the decision (along with Jim’s sisters and mother) to take part in the study after they were approached by Alan Spriggs of Legacy of Hope and Locke.
“Jim was a never-met-a-stranger kind of guy who would talk to anyone and had no enemies – none,” O’Hara said. “Jim would have wanted to save as many people as he could with his death, and if he knew he could potentially save thousands and thousands of people by doing this, he would have had no hesitation. Our dream is that no other person dies waiting for a kidney, and we know that Jim is very proud that his death could potentially bring so much hope to others.”
(UAB videography by Jeff Myers and Steve Wood)
To learn how to become a registered organ donor, visit Legacy of Hope’s official website.
The critical need for other organ donation options
Kidney disease kills more people each year than breast or prostate cancer, according to the National Institute of Diabetes and Digestive and Kidney Diseases. Although transplantation is the gold standard treatment for end-stage kidney disease, fewer than 25,000 kidney transplants are performed each year in the United States and 240 Americans on dialysis die every day. Many of these deaths could be prevented if an unlimited supply of kidneys were available for transplant.
The wait for a deceased donor kidney can be as long as five years, and in many states, it is closer to 10 years. Almost 5,000 people per year die waiting on a kidney transplant.
About UAB transplant and the xenotransplant team
UAB Medicine is a world leader in organ transplantation and performed 9,055 kidney transplants from Jan. 1, 1988, to Dec. 31, 2021 – the second-most kidney transplants in the United States during that time. The focus of UAB’s xenotransplantation program is to address the organ shortage by safely transplanting genetically modified pig kidneys into humans with kidney failure. Learn more.
This story originally appeared on the UAB News website.






